Soft tissue grafting procedures have long been used to help manage gingival recession defects. Initially, the approach was to use autogenous, full-thickness, palatal soft tissue grafts to increase the width and thickness of keratinized tissue to minimize the progression of recession and improve patient comfort.1 Subsequent introduction of the de-epithelialized, palatal connective tissue graft (CTG) led to the extensive development of gingival periodontal plastic techniques to achieve partial or complete soft tissue root coverage at existing recession defects.2 Various operative techniques have been proposed, the most common being the combination of CTGs with coronally advanced gingival flaps3 or using “tunnelling” to introduce CTGs without actual flap reflection.4 These approaches are now considered “standard of care.”
CTGs are generally effective at isolated gingival recessions. Still, many patients have multiple defects that could benefit from the procedure but insufficient donor tissue to treat them in single surgical sessions. As a result, the industry has developed CTG substitutes and promoted them for this purpose. One type of substitute is the acellular dermal matrix (Alloderm®, Biohorizons Inc.), a chemically processed allograft from which all epidermal and dermal cells have been eliminated, leaving only a scaffold of collagen, elastin, blood vessel channels, and claimed to have bioactive proteins supporting natural revascularization and cell repopulation. The preferred approach with this type of material is to use tunnelling of the tissues surrounding recession defects to create protected recipient sites for ADM. Results from a recent publication comparing tunnelling with ADM versus autogenous connective tissue showed that somewhat similar outcomes could be achieved with both when used in managing multiple adjacent recession defects.5 Nine months post-surgery, significant improvements in gingival recession depth, gingival recession width, gingival thickness (GT), keratinized tissue width KTW), probing pocket depth, clinical attachment level, and percentage of root coverage were seen with both materials. The significant differences were that the CTG group showed more KTW gain (P = .0003) and greater GT (P = .002) than the ADM group. However, there were no differences in patient esthetic satisfaction recorded using a visual analogue scale. The paper presents a recent case of multiple adjacent substantial gingival recessions treated with ADM using a vestibular incision and subperiosteal tunnelling (VISTA®).6 The VISTA® approach was proposed by Zadeh et al. in 2011 to provide access for the insertion of a soft tissue graft via tunnelling through a vestibular incision circumventing significant trauma to the marginal gingiva.6
Materials & Methods
The patient was a healthy, 59-year-old non-smoking female who presented with generalized RT2 and RT37 recession defects affecting most of her maxillary teeth. She wished to have soft tissue grafting for the ten teeth from the second bicuspid to the second bicuspid. (Fig. 1) She requested that the least number of surgical procedures be done and declined to have autogenous soft tissue grafting, preferring the option of an allograft material. The treatment goal was to increase the amount of keratinized tissue and improve esthetics. Root coverage was not a goal of treatment as mild/moderate interdental bone loss was present in the proposed sites.
Fig. 1

On the day of surgery, the teeth undergoing treatment were thoroughly scaled and root planed with Gracey curettes and fine Piezo tips. The composite restorations were partially removed and polished to obtain smooth and slightly concave surfaces. Complete removal of restorations was contraindicated due to the risk of pulpal exposures. The teeth were then rinsed thoroughly with sterile saline.
As depicted in Fig. 2A, a 6-mm-long vertical incision was made using a #15c scalpel blade at the midline between the two central incisors in the maxillary alveolar mucosa starting at the mucogingival junction and extending apically. Bilateral, full-thickness tunnelling was initiated using an Allen end-cutting intrasulcular knife and a 4R/4L Columbia Universal curette and further developed using Allen anterior and posterior periosteal elevators. Ultimately, this tunnelling released the marginal gingiva of ten affected teeth. Further tension-free releases apically and interdentally underneath the interdental papillae were achieved using 7/8 Younger-Good curettes and the Allen end-cutting intrasulcular knife. Ultimately, the tunnel extended from the first molar to the first molar, i.e., one tooth distal to the large surgical site. While the distal papillae of both first bicuspids were released, all other papillae remained intact.
Fig. 2A

Having prepared the surgical bed, a piece of Alloderm® (1cm x 4cm) was aseptically rehydrated in sterile saline following the manufacturer’s instructions, cut horizontally into two halves, and adjusted to fit the recipient sites. A 4-0 chromic gut suture needle was inserted into the tunnel distal to one first bicuspid and advanced mesially to emerge from the midline VISTA® incision. Half of the allograft was then engaged with the needle, pulling it distally through the tunnel to cover the surgical bed. (Fig. 2B) Similar steps were repeated for the contralateral side, after which both allograft halves were fitted to cover the exposed root surfaces up to the cementoenamel junction (CEJ) of each tooth and the surrounding bone. (Fig. 2C) Multiple interrupted sling sutures using 6-0 prolene captured both the buccal flaps and allograft segments to optimize graft stability. The midline VISTA incision was closed using 5-0 chromic gut single interrupted sutures. Finally, the flaps were sutured without tension, ensuring no intraoral exposure of the allograft material. (Fig. 2D & E) Gentle pressure with moist gauze was applied over the surgical site for 3 minutes, after which flap immobility was verified by stretching and moving the lips.
Fig. 2B
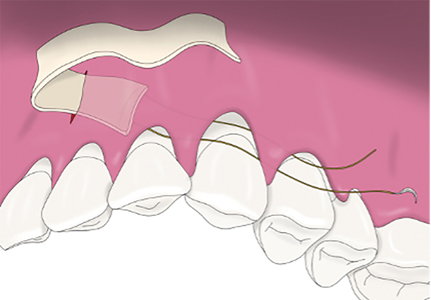
Fig. 2C
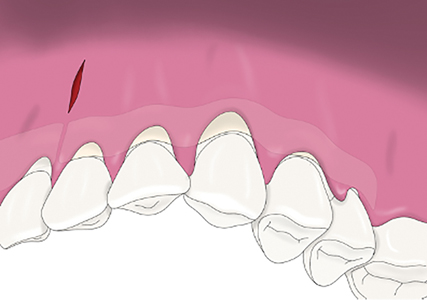
Fig. 2D
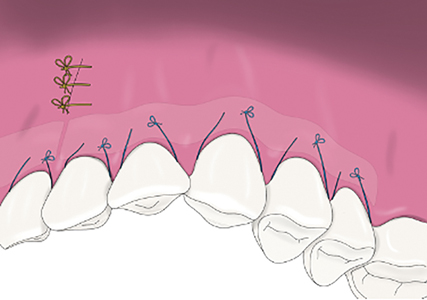
Fig. 2E

As the patient was allergic to penicillin, azithromycin 250mg was prescribed as two tabs immediately followed by one tab/day for days 2 to 5. Ibuprofen 600mg was prescribed for analgesia every 6 hours as needed. Other instructions included using bidaily, gentle saltwater rinsing, a soft diet for three weeks, and no brushing of the recipient for two weeks.
Post-operative photos were taken immediately post-op, (Fig. 2E), at one week, (Fig. 3) three weeks at suture removal, (Fig. 4) then two months after surgery. (Fig. 5) No exposure of allograft material or signs of infection were detected throughout the healing period. One week post-op, the patient reported having had mild discomfort immediately after surgery and for the following 2-3 days.
Fig. 3

Fig. 4

Fig. 5

Conclusion
Soft connective tissue grafting has been shown to have positive, predictable outcomes in root coverage procedures. However, autogenous grafting requires a second surgical site and may not be possible or desirable for some patients. Fortunately, allograft materials such as acellular dermal matrix (ADM) can be used as alternatives. In the present case report, the VISTA® approach was used with ADM to successfully treat multiple adjacent maxillary gingival RT2/RT3 recession defects.
Oral Health welcomes this original article.
*Corresponding Author: douglas.deporter@dentistry.utoronto.ca Orcid account # https://orcid.org/0000-0003-2531-8747 Tel: 416-864-8208; FAX: 416-979-4755.
Mailing Address: Discipline of Periodontology, Faculty of Dentistry, University of Toronto, 124 Edward Street, Toronto, ON, Canada M5G 1G6.
References
- Miller Jr., P. D. Root Coverage with the Free Gingival Graft. J Periodontol 1987, 58 (10), 674–681. https://doi.org/10.1902/jop.1987.58.10.674.
- Zucchelli, G.; Amore, C.; Sforza, N. M.; Montebugnoli, L.; De Sanctis, M. Bilaminar Techniques for the Treatment of Recession-Type Defects. A Comparative Clinical Study. J Clin Periodontol 2003, 30 (10), 862–870. https://doi.org/10.1034/j.1600-051x.2003.00397.x.
- Langer, B.; Calagna, L. The Subepithelial Connective Tissue Graft. J Prosthetic Dent 1980, 44 (4), 363–367. https://doi.org/10.1016/0022-3913(80)90090-6.
- Zabalegui, I.; Sicilia, A.; Cambra, J.; Gil, J.; Sanz, M. Treatment of Multiple Adjacent Gingival Recessions with the Tunnel Subepithelial Connective Tissue Graft: A Clinical Report. Int J Perio Rest Dent 1999, 19 (2), 199–206.
- Elmahdi, F.; Reda, A.; Hosny, M. Evaluation of Subepithelial Connective Tissue Graft Versus Acellular Dermal Matrix with Modified Coronally Advanced Tunnel Technique in Treatment of Multiple Gingival Recessions: A Randomized, Parallel-Design Clinical Trial. Int J Perio Rest Dent 2022, 42 (6), 741–751. https://doi.org/10.11607/prd.5522.
- Zadeh, H. H. Minimally Invasive Treatment of Maxillary Anterior Gingival Recession Defects by Vestibular Incision Subperiosteal Tunnel Access and Platelet-Derived Growth Factor BB. Int J Perio Rest Dent 2011, 31 (6), 653–660.
- Cairo, F.; Nieri, M.; Cincinelli, S.; Mervelt, J.; Pagliaro, U. The Interproximal Clinical Attachment Level to Classify Gingival Recessions and Predict Root Coverage Outcomes: An Explorative and Reliability Study. J Clin Periodontol 2011, 38 (7), 661–666. https://doi.org/10.1111/j.1600-051X.2011.01732.x.
- Do, J.; Latimer, J.; Nguyen, T. Multiple Subperiosteal Sling Sutures for Connective Tissue Graft Stabilization in the Treatment of Multiple Recession Defects Utilizing Subperiosteal Tunnels via VISTA and Intrasulcular Access. Int J Perio Rest Dent 2023, 43, 379–385. https://doi.org/10.11607/
About the Authors

Sonia Ruo Chen Huang is a 2023 graduate from the Discipline of Periodontology, Faculty of Dentistry, University of Toronto, former Periodontic Resident, practicing in British Columbia.

Rickson Valtellini is a first-year Periodontic Resident in the Faculty of Dentistry, University of Toronto.

Dempsey Wood is a first-year Periodontic Resident in the Faculty of Dentistry, University of Toronto.

Ryan Noh is an Assistant Professor of the Discipline of Periodontology the Faculty of Dentistry, University of Toronto and maintains a part-time, private practice in Waterloo, ON. He is also a highly sought-after medical illustrator.

Douglas Deporter is a Professor of the Discipline of Periodontology Faculty of Dentistry, University of Toronto, Co-Inventor of the Endopore® dental implant system, researcher, international speaker, and widely published author. His latest book, “Immediate Molar Implants, “ was published by Quintessence Int in 2023.